The number one trend affecting all businesses is digital transformation. The metamorphosis of expectations are being driven by companies like Amazon, Apple, Netflix, DoorDash, and Venmo, that offer transparent, immediate, and embedded payments experiences. Consumers have embraced fully digital interactions, which are laying bare the shortcomings of non-digital experiences such as paper billing and check payments.
Of course, the pandemic is driving more customers to digital transactions. What the industry was expecting to evolve over the next 1-3 years has instead increased in momentum in the last year.
As a result, it’s time to look at the end-user not just as a policyholder, but as a customer. In a recent webinar, experts from Aite Group and Alacriti discussed how digital innovation is reshaping payments in the insurance industry. This article explores this topic further.
Quick Links
Digital payments and contactless payments are not new technologies by any means, but the speed of adoption and customer expectation has accelerated. For instance, digital payment transactions are expected to hit $6.7 trillion in 3 years — a gain of 63% from 2019 (Statista).
These current trends have accelerated the need for insurers to implement digital payment technologies. This is especially significant considering payments are one of the most frequent interaction points between insurers and policyholders. As a result, it’s time to look at the end-user not just as a policyholder, but as a customer. In a recent webinar, experts from Aite Group and Alacriti discussed how digital innovation is reshaping payments in the insurance industry. In this article, we will also cover this topic.
Billing and Payments
The easiest bill to pay gets paid first. There are a lot of important transformational activities taking place across the insurance value chain, such as claims automation, underwriting, distribution, etc. The automation of payments processing is becoming increasingly important. According to Mike Trilli, Insurance Practice Research Director at Aite Group, the most important digital transformation trend from an insurance standpoint is payments processing.
On the P&C side, there is a focus on automation improving the customer experience. Billing and payments innovation drives efficiency savings, increased loyalty and retention, and overall satisfaction. On the healthcare side, the term isn’t necessarily ‘digital transformation’ but, the goals are the same. They’re investing in reengineering their patient receivables, their payables process, and disbursements. This is especially important with the increase of third-party payers, which drives the need for stronger relationships and a frictionless process and experience. In short, carriers and healthcare providers are trying to connect more with people that are paying for services for them.
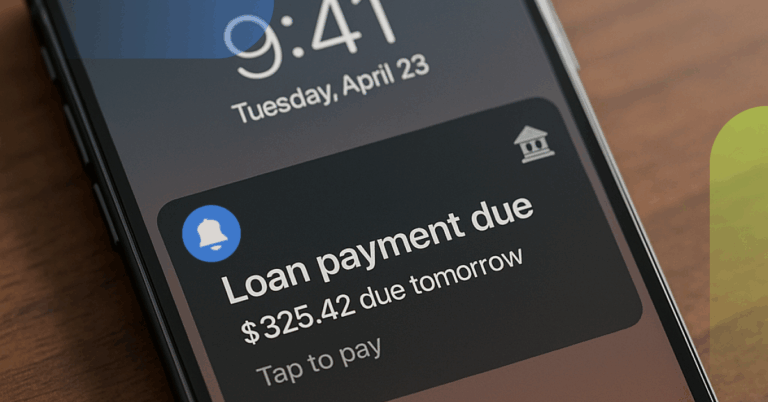
To Jay Sarzen, P&C Insurance Practice Sr. Lead at Aite Group, the insurance industry is viewing policyholders as customers now, which has led to the emergence of payment choice. Policyholders have multiple options to pay, which is not innovative in general, but for the industry it’s true progress. The introduction of a more intuitive user interface is even more of an improvement, allowing users to pay via text, online, over the phone, etc. For P&C, there is a real appetite to have one point of reference for everything. Many carriers have multiple lines of business, and they want to provide one interface to accommodate them. Also, the use of paper checks is dwindling. In the past, insurance companies were happy to issue a paper check, but now they’re realizing that paper checks are an arduous and expensive process. They now know that the way to keep customers happy is to provide payment and disbursement options. Now carriers offer push to debit, payment to a credit card, payment to a virtual card, etc. But the arrival of The Clearing House’s Real-Time Payment network as an alternative to the standard ACH rail is also in play.
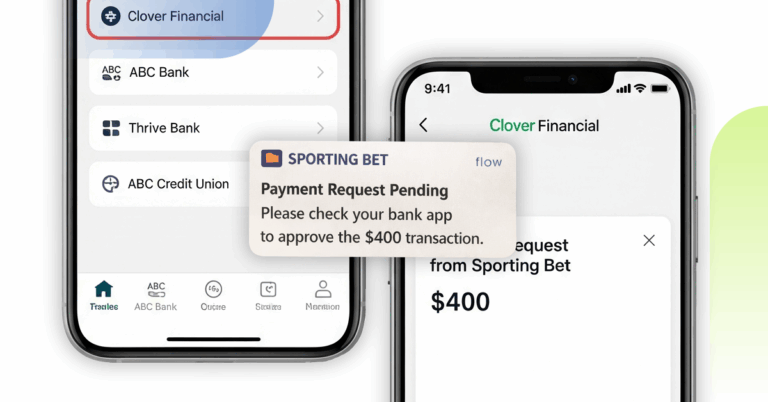
Stuart Bain, SVP of Product Management at Alacriti, recommends that the payments experience be consistent on every channel. For example, insurers are starting to provide kiosks so that staff doesn’t have to handle cash payments. It also integrates cash (using a barcode) into the web experience, which is a much more seamless process. New options like request to pay through the RTP® network and MasterCard Bill Pay Exchange will allow the payments experience to extend to online banking. Consumers can pay their bills with real-time payments from their bank accounts and receive confirmation, all within their banking app or banking website.
Cutting edge experiences like progressive web apps also benefit insurance companies. Progressive web apps were created to counteract consumer app fatigue and combine the best of the web and the best of native apps. This allows for a more app-like experience, e.g., offline notifications, without having to install an app on your device. For instance, some insurance companies require users to sign up on the company’s portal to make a payment online, but a Guest Pay option makes for a better experience for those that don’t want to mail in a payment but also don’t want to sign up on yet another website.
Artificial Intelligence and Chatbots
According to Jay Sarzen, P&C Insurance Practice Sr. Lead at Aite Group, AI has a broad application across the insurance value chain. In underwriting, it can be used for your initial data intake for insurance policies, analyzing and incorporating unstructured data like photos or weather data. In claims, a chatbot can be used for automated first notice of loss. Chatbots can take basic data from a person that suffered a loss, and AI can structure it in a way that ensures the correct adjuster is assigned. This is a key win to avoid significant delays in claims processing typically attributed to incorrect claim adjuster assignment, which is a common challenge. For payments, AI is a useful analytics tool for fraud prevention to guard against claimants using false identities. The cost of insurance fraud is more than $40 billion per year. Using AI to detect abnormalities in claims data and identify false information that can be fraudulently used to get lower premiums or bigger payouts is a key use case.
Stuart Bain at Alacriti has noticed that chatbots are most commonly used to manage call center volume, particularly since COVID-19 exposed issues with call center capacity. There are three types of inquiries that chatbots can handle:
Generic questions that can usually be answered from website information, where the answer will be the same no matter who asks the question, e.g., what are your call center hours?
Payment intake queries where chatbots are set up like a CSR to provide information about the bill and accept payments.
Account-based questions, which provide policy-specific data, e.g., what is my remaining deductible?
The purpose of deploying a chatbot to manage these types of common queries helps to reroute these types of calls from the call center so the CSRs can answer more complex questions while the caller can get their question answered more quickly.
Before implementing a chatbot, you have to make sure that your culture is aligned and there’s executive buy-in. Then assess your level of readiness, considering there are different levels of automation:
1
Class 1
automation is a chatbot that can do an intake of basic information and provide pre-packaged responses.
2
Class 2
automation leverages the AI component to allow the chatbot to make some decisions. For example, the chatbots can handle claims that are less than a certain dollar amount.
3
Class 3
automation also referred to as “hyper-automation” where the chatbot is empowered with full analytics capability using AI and machine learning. For example, the chatbot can make meaningful decisions about what might have happened in an accident (accident reconstruction) or insight into overall risk/ underwriting decisions.
Once a decision has been made, it’s practical to assure employees that the AI chatbot is not a displacement tool, it’s an enhancement tool.
AI has a broad application across the insurance value chain:
- In underwriting, it can be used for your initial data intake for insurance policies, analyzing and incorporating unstructured data like photos or weather data.
- In claims, a chatbot can be used for automated first notice of loss.
- For payments, AI is a useful analytics tool for fraud prevention to guard against claimants using false identities.
Digital Disbursements
A claim payment is seen as the most impactful event in the insurer-insured relationship. Digital disbursements can create a level of engagement that can’t be achieved with a check-based payment. When asked about modernization, Mike Trilli, Insurance Practice Research Director at Aite Group, believes that a core aspect of modernization is evaluating paper-based and manual interactions and how to modernize from a digital standpoint. Another key element of modernization is choice. The policyholder should be able to have some level of choice about the method they want to receive the disbursement. With Aite research, Trilli states, this was the most important element of modernization from a consumer perspective. Delivering and settling funds quicker is another component of modernization. COVID-19 has increased the pressure to provide a better service experience. For example, Allstate® streamlined their process and removed friction points, and saw a bump in customer satisfaction and retention.
Aite’s Jay Sarzen came across interesting information when researching why carriers like paper checks. Carriers feel that paper checks: offer low complexity, guarantee any data associated with it is largely safe, satisfy regulators, and provide the ability to verify whether or not a payment has been completed with a returned check. Having money an extra day or two (float) was also listed but as a minor reason. Carriers need not abandon checks altogether, but they should make sure that their customers have choices. Sarzen’s research demonstrated that every one of the digital payment options provided (ACH, Same Day ACH, virtual debit card, physical debit card, reloadable gift card, alias-based payments like Venmo, Paypal, ora credit card) is equivalent to the paper check in terms of low complexity, data safety, ability to verify, etc. The only area where digital payments fall short is on the float aspect as real-time payments don’t allow for float, however, research indicates it’s not a chief concern.
Another thing to keep in mind is that speeding up payments creates a decrease in payment inquiries. Mark Ranta, Payments Practice Lead at Alacriti, advises insurance companies to look at the experience holistically. When you examine the experience from the point of claim initiation to payout, an automated and digitally harmonious experience can lower the inbound calls, avoid unnecessary pain, and make the payment easier while limiting the possibility of fraud.
The policyholder should be able to have some level of choice about the method they want to receive the disbursement. With Aite research, Trilli states, this was the most important element of modernization from a consumer perspective.
Real-Time Payments
In 2017, The Clearing House introduced a new central infrastructure and new rail for money movement in the U.S. called the RTP network. It’s the first new central and clearing and settlement network to hit the market in nearly four decades. That may be surprising to some considering major new systems like Zelle and Venmo, however, these are overlay systems that rely on existing infrastructure.
The introduction of the RTP network is the first step for payments modernization in the U.S. Changing payments habits and real-time adoption have been somewhat slow for the first few years. However, the network is now capable of reaching over 60% of all U.S. DDA accounts. As more banks connect to the network, we can expect real-time payments to be more prevalent in the market. This means that consumers will start seeing real-time payments for the first time. Many consumers erroneously think that they DO have real-time payments, but really, they have overlays that made the experience real-time, but the actual money movement is not.
In the next two years, there will be a new network going online from The Federal Reserve — FedNow Service. There are also a handful of systems going online in the next few years. Mike Trilli from Aite recommends that insurers understand where the market is headed and extend into new payment options. This is a time of learning and testing. It’s a great time for insurers to identify the segment of the population that are primed for new options and start testing.
Property & Casualty is very different from Health Insurance in that, outside of workers’ compensation, claim payments are much less frequent than medical disbursements. Aite’s Jay Sarzen has seen statistics that show 60-65% of all claimants (even after that they’ve been made whole by the carrier), will consider switching carriers because the process was too arduous or it just didn’t meet their expectations. Carriers are recognizing that payments are a customer interaction that shouldn’t be an afterthought. Instead, they should think of it as a retention tool in a relationship that does not facilitate many interactions outside of payments to impress and show value to customers.
As insurance companies seek vendors to assist with their digital transformation, they should look for continual improvement. The vendor should constantly look at new and emerging payment channels and methods to ensure the most modern experience for your policyholders. Also, they should try to reduce payment processing costs while helping insurers generate revenue.
Alacriti’s centralized payment platform, Orbipay Payments Hub, provides innovation opportunities and the ability to make smart routing decisions at the financial institution to meet their individual needs. Financial institutions can take full ownership of their payments and control their evolution with ACH, Wire, TCH’s RTP® network, Visa Direct, and the FedNow® Service, all on one cloud-based platform.